Disease Carriers and their diseases
Poverty was a major cause of heavy outbreaks of disease, with many people living on the edge of subsistence, having a minimum of warmth, clothing, and shelter, and with the ever-present threat of starvation hanging over their heads. It is not surprising, therefore, that bodies weakened by malnutrition readily succumbed to diseases such as typhus, tuberculosis, and smallpox. We shall now look at the various kinds of disease carrier and the diseases they caused.
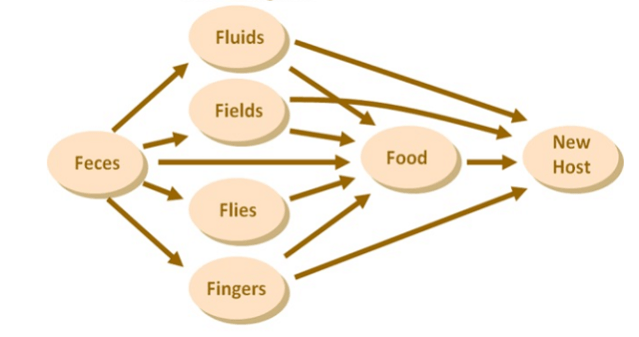
The main carriers of disease can be classified as follows:
Mechanical Vectors
These are any objects or substances that are capable of carrying infectious organisms but where the disease does not replicate or develop either within or on the vector. The vector simply acts as a means of transport. The air, for example, may transmit organisms from one person to another, tuberculosis and influenza being two cases in point, where the bacteria and viruses respectively are spread as aerosol droplets through the air.
Recent research has shown, that coughing and sneezing creates a fine mist of pathogen rich mucosalivary droplets which can be released at a speed of between 33 to 100 feet per second (10-30 m/s), can cover a distance up to 23 to 27 feet (7-8 m), and remain airborne from a fraction of a second to several minutes.
Water can also serve as a means of transporting disease carrying organisms. Perhaps the two most well-known of these are typhoid, caused by the bacterium, Salmonella typhi, and cholera, which is caused by the comma-bacillus, Vibrio cholera. Both of these organisms are transported mainly by unhygienic water supplies, although insect vectors may occasionally be involved.
A third mechanical vector is contaminated food. Improperly preserved foods, for example, may harbour the extremely fatal toxin, Clostridium botulinum, which is one of the most powerful toxins known. In 2011, food contaminated with the bacterium E-coli, was responsible for the deadliest outbreak of bacterial food poisoning in Germany as well as in Europe, and this resulted in the deaths of 53 people, having infected more than 3,950.
Human Vectors
Human beings may carry disease from one to another, smallpox and tuberculosis being notable examples. In addition, some people, having recovered from a disease, become carriers of that disease. About 30% of surviving typhoid cases become carriers, excreting the bacterium in their faeces and urine for several weeks, with about 5% becoming long-term carriers, harbouring, and shedding the organisms for many years.
Animal Vectors
Whilst perhaps the most widely known of these is the black rat, which may, under certain conditions, be a plague carrier, various other animals may also harbour diseases which are caught by human beings. Cattle, sheep, goats, pigs, deer and rabbits are all natural reservoirs of brucellosis; milkmaids used to catch cow-pox from the udders of infected animals, and bovine tuberculosis can be caught by drinking unpasteurised milk from infected cows. Recent research by Zhiqiang Wu and colleagues has found bats housing 79 virus families including 19 which affect mammals. These do not appear to harm the bats as they appeared healthy and disease free.
Bats are able to spread their virome in four ways: by air, droplet, oral-faecal indirect contact and direct physical association. As several diseases such as Ebola, Marburg and SARS have been blamed on bats, it is tempting to surmise whether these animals could have been agents of disease during the Early Modern period. In this context we should mention SARS-CoV-2, the pathogen responsible for Covid-19, which may have been spread from bats to other animals and from them, to the human food chain. However, there is a school of thought that thinks, not without good cause, that the virus was an escapee from a research laboratory in Wuhan.
Insect Vectors
Insect vectors are far more important than animals in this respect. Body lice (Fig. 1) are the carriers of typhus which is carried in their faeces which are then either scratched into small abrasions or inhaled, thus causing the infection.

Houseflies (Fig. 2), blue bottles (Fig.3), green bottles and cockroaches (Fig. 4), which feed upon refuse, faeces, decaying filth and human food, are known to harbour huge quantities of pathogens, whilst some species of mosquitos carry malaria, amongst other diseases, and black rats and various other rodents can harbour fleas infected with bubonic plague.



Flies are hosts to several hundred species of pathogenic organisms and are believed to transmit at least 65 diseases to both animals and humans. It also reported that in a study carried out in Beijing, on a total of 384,193 flies that had been caught, it was estimated that those from a slum area carried 3,683,000 bacteria each, whilst those from the cleanest area, 1,941,000. Writing about outdoor defecation in the third world in the August 2017 edition of the National Geographic Magazine, Elizabeth Royte said that:
Flies breeding and feeding on faeces are one of the main vehicles delivering infectious organisms back to humans: 1 gram of faeces can contain 10 million viruses, 1 million bacteria, and 1,000 parasitic cysts, which infect us through minute openings in our skin or by contaminating food and water.
Diseases
The range of common diseases that anyone living in the 18th century was likely to encounter was large by present day standards, and unfortunately, as the medical profession was ill-equipped to deal with them, death was never far away. Fear of contagion must have been ever present. A simple cut or broken bone might be the harbinger of an infection such as sepsis, tetanus, or gangrene, which, without the benefit of modern antibiotics, would lead ultimately to death. Recent research that was published in the Lancet in January 2020, estimates that even today, one in five deaths around the world is caused by sepsis. One therefore has to wonder, what the percentage would have been in the 18th century.
Bacillary dysentery or Shigellosis
Bacillary dysentery or Shigellosis is caused by one of four species of Shigella, namely: Shigella sonnei, Shigella flexneri, Shigella boydii or Shigella dysenteriae. However, the virulent and potentially fatal form of the disease is caused by the organism, Shigella dysenteriae, which is the only one of the four species of Shigella capable of causing a major epidemic. In the developing world, the fatality rate can be as high as 30%. In severe forms of the disease the patient passes bloody stools at the outset, and becomes toxic and restless, with a rapid feeble pulse, and death may result from circulatory failure or haemolytic uraemic syndrome. Other symptoms include abdominal pain, cramps, fever and vomiting. The principal method of transmission of the disease is by direct faecal-oral spread of bacteria via contaminated, fingers, whence it is conveyed to food such as salads, poultry or raw vegetables. It may also be transmitted by flies which have alighted on exposed human faeces, and large outbreaks have occurred through faecal pollution of water supplies.
Bronchitis
Bronchitis is an inflammation of the bronchi of which there are two types, acute and chronic. Acute bronchitis is usually caused by a viral or bacterial infection which can develop after a cold or influenza. It can also be caused or exacerbated by various forms of air pollution and smoke. Symptoms include sore throat, wheezing, chest pain, fatigue, fever, aching body, stuffy or runny nose, vomiting, and diarrhoea. However, the main symptom is a persistent cough, which may last about 3 weeks. Even after the infection clears up, there may still be a dry cough which lingers for days or weeks.
The signs and symptoms of chronic bronchitis, which is defined as lasting for 3 months or more, include coughing, wheezing, and chest discomfort. The coughing may produce large amounts of mucus. It is particularly prevalent amongst people who are continually exposed to dust and fumes, and it may be aggravated by high concentrations of sulphur dioxide or other pollutants in the air.
Brucellosis
This is a generalised infection of humans caused by one of four species of Brucella, namely: Brucella melitensis, Brucella abortus, Brucella suis and Brucella canis. The disease is transmitted by direct or indirect contact with the natural animal reservoirs, especially, cattle, sheep, goats, pigs, deer and rabbits, or their infected products or tissue, the usual method of infection being unpasteurised milk.
Other symptoms not mentioned may include chest pain which is worse on breathing, palpitation due to an arrhythmia, abdominal pain with constipation, and confusion with nightmares and somnambulism. High fever is usual, and the spleen is often enlarged and the liver palpable.
An infection from B. abortus can be life-threatening especially when resistance is low. If the disease takes on a chronic form, changes in the skeleton may occur, due to reactive arthritis, with the large joints and spine being particularly affected. Such changes make it possible to diagnose this disease in skeletal remains.
Although a debilitating disease, mortality in brucellosis is very low, certainly less than 5% and probably less than 2%. It is usually the result of the rare instance of Brucella endocarditis or of severe CNS (central nervous system) involvement, often as a complication of endocarditis. Other fatal complications include, myocarditis and pericarditis.
Common cold
As the saying goes, “Coughs and sneezes spread diseases”. However, when their symptoms could presage such fatal diseases as plague, an all too recent memory in the minds of some, and fevers of various kinds, which could kill within a short time, they were looked upon not so much as afflictions in themselves, but as forerunners of something far more serious.
The common cold virus, – and there are well over 200 implicated in the transmission of this disease – is spread through the air by aerosol transmission, direct contact with infected secretions but mostly by fomites, especially hand to hand contact. Henri Misson, a French visitor to England at the end of the seventeenth century wrote in his “Mémoires et observations faites par un voyageur en Angleterre”:
Rhumes. Un Rhûme qui s’invétére en Angleterre, est un commencement de maladie mortelle, particulierement pour les Etrangers. Il ne faut donc pas negliger en rhûme.
Colds. A long-lasting cold in England is the beginning of a deadly illness, particularly for strangers. It’s not wise, therefore, to neglect a cold.
Diphtheria
Diphtheria is a potentially fatal highly contagious bacterial infection that mainly affects the nose and throat, and sometimes the skin. It is caused by toxigenic strains of two types of bacteria, namely: Corynebacterium diphtheriae and Corynebacterium ulcerans It is usually confined to the upper respiratory tract and is characterized by a tough false membrane attached firmly to the underlying tissue which bleeds if removed by force. It may spread throughout the throat, larynx and bronchial tree where it may cause death by hypoxia. Diphtheria which is mainly an autumn disease is spread by coughs and sneezes, by direct contact with someone who has the illness or by objects that they have handled.
Ergotism and other forms of Mycotoxicosis
Ergotism
There are two forms of ergotism which are caused by the fungus, Claviceps purpurea (Figs. 5 & 6), namely, gangrenous and convulsive. Victims of the gangrenous form may lose hands, fingers, toes, or even complete limbs, whilst victims of convulsive ergotism suffer tonic/clonic seizures such as writhing, tremors and wry neck and in severe cases, coma and death.


The contamination of grain with ergot (Claviceps purpurea) has spread death and destruction for thousands of years. An ancient Assyrian tablet, circa 600 BC, referred to the “noxious pustule in the ear of grain”, and around 350 BC, one of the sacred books of the Parsees mentions “noxious grasses that cause pregnant women to drop the womb and die in child bed”.
Ergotism can be a very lethal disease. For example, during ten epidemics recorded in Russia from 1832 to 1864, between 11% to 66% of those who became sick died, with a mean mortality rate of 41.5%.
Favourable conditions for the formation of Claviceps on rye occur if the preceding winter is cold, there is a wet and cloudy spring which lengthens the time the rye flowers are open, and the temperature is between 17.4° and 18.9°C. These weather conditions may also be favourable for insect populations of aphids, thrips, midge and leaf hoppers, which serve as potential vectors of sticky spores, thus spreading the infection.
Ergotism epidemics usually occur from late summer onwards after the rye harvest, when ergot is at its most toxic, but can occur at any time as the Claviceps alkaloids are able to remain viable for up to eighteen months.
There is a possibility that the dry fog produced by the Laki eruption caused the favourable conditions necessary for the production of ergot by blocking out the sunlight and thus maintaining a constant humidity, thereby allowing Claviceps purpurea to thrive. However, ergot poisoning, even if not fatal, may also affect the fertility of the population. This may be inferred by the drop in conceptions in August and September, after the harvest.
Aspergillosis
Aspergillosis is a fungal infection caused by various species of Aspergillus, but usually Aspergillus fumigatus. A. fumigatus is the most common airborne fungus due to growth in a wide range of temperatures and is commonly found on rotting vegetation, dead leaves, compost heaps and stored cereals. Like all moulds, it likes damp conditions, and is thermotolerant, its optimum temperature for growth being between 37 and 43°C. The metabolites that this fungus manufactures can cause tremors and convulsions in men and animals, and as some of its metabolites are the same as those of ergot, it may, in addition, also produce hallucinations. It might well be that Aspergillus and not ergot has caused some of the epidemics in the past.
Alimentary toxic aleukia (ATA)
This is a very severe form of toxicosis caused by trichothecenes such as T-2 mycotoxin, which have been produced by Fusarium tricinctum. It is an exceptionally nasty disease, causing amongst other things, fever, vomiting, haemorrhaging from the skin, nose, throat and gums, necrosis, ulcerative sore throat and leukopenia. These features are similar to radiation poisoning, and quite different from those caused by most other bacterial or. mycotoxins. ATA was identified as being the cause of some 100,000 deaths between 1942 and 1948 in the Russian grain belt, the death rate in some cases being as high as 60%. In this particular case, the toxin was produced in grain that was overwintered in the fields and not harvested until the following year. Although the toxin starts to form in the autumn, it only reaches its maximum toxicity in the spring, particularly if there has been abundant snow with alternate freezing and thawing. The optimum temperature for its formation was thought to be between 5° and 14°C.but this has now been revised upwards to 25°C.owing to a strain of Fusarium toxin that was produced at this temperature in South Africa. As well as overwintering in fields, grain which has over 16% moisture is particularly liable to infection, but if it stored with a moisture content of less than 13°C.it will not be liable to mould growth, a situation I think most unlikely to have happened in eighteenth century Europe.
Not only is this toxin an extremely strong poison, but it is also a potent immunosuppressant. It causes irreversible damage to the bone marrow, leading to characteristic reduction in white blood cells (leukopenia). Although continued consumption of T-2 toxin will ultimately lead to death, it is thought that many of the fatalities during these outbreaks of ATA probably occurred due to viral and bacterial infections with which the victim’s defective immune systems were unable to cope.
It is quite possible, that in the past, what we now know to be ATA was mistaken for diphtheria or a combination of scarlet fever and diphtheria. However, with ATA no false membrane forms in the throat as it does with diphtheria, whilst scarlet fever is characterised by a high fever, sore throat and a sandpaper-like red rash, but no ulcerated throat or haemorrhaging.
Infantile diarrhoea
According to the 2014 UNICEF Report, Levels & Trends in Child Mortality, 9% of deaths of all children under five are caused by infantile diarrhoea, thus making it one of the leading causes of mortality in children in this age group. This highly infectious disease is caused by a rotavirus which is transmitted by the faecal-oral route, either directly through contaminated hands, or indirectly via food, utensils, soil, flies, or contaminated drinking water. Fig 7
If this disease is a leading killer of young children under five today, I see no reason to doubt that it had the same effect during the 18th century, especially when considers the unclean living conditions that the majority of the population had to tolerate.
Influenza
Influenza is usually spread by person-to-person transmission through the transmission of aerosol sized particles generated by coughing, sneezing or talking. It can also be transmitted through the handling of objects that are contaminated by the virus. The main symptoms include: high fever, runny nose, sore throat, muscle pains headache, dry cough, tiredness and shivering. Unfortunately, acute influenza may transform into either primary or secondary pneumonia, which can lead to an extremely high rate of mortality. The following table illustrates how an influenza epidemic spread throughout Britain in 1782, beginning in Torrington, North Devon in the south-west of England on 24 March and by the time it had finished in October had covered the majority of England and a large part of Scotland.
The British 1782 influenza epidemic
| Year | Town | Start of infection | End of infection |
| 1782 | Torrington, North Devon | 24 March | Before June |
| Newcastle | End of April | Mid-June | |
| London | 12th-18th May | ||
| Eastern Counties | Mid-May | ||
| Surrey, Edinburgh, Portsmouth, Oxford Chester | 3rd week of May 26th May | July | |
| St. Albans | Before 28 May | ||
| Plymouth | 30th May | ||
| Ipswich, Yarmouth, York, Liverpool Glasgow | 1st week in June | ||
| Barnstable | June | ||
| Musselburgh | 9th June | ||
| Northumberland | July | 3rd week of August | |
| Scotland | July height of epidemic | ||
| Gravesend | September | ||
| London | Beginning October | Both this and the Gravesend outbreaks were unusual occurrences |
An indication of how quickly the disease could spread is given in the following extract from Vol. 2 of Charles Creighton’s “A History of Epidemics in Britain”.
… two months after the late epidemical catarrh had entirely disappeared from England. The king’s ships ‘Convert’ and ‘Lizard’ arrived in the Thames from the West Indies in September. Their crews were perfectly healthy till they reached Gravesend, where they took on board three custom-house officers; and in a very few hours after that the influenza began to make its appearance. Hardly a man in either ship escaped it; and many both of the officers and common seamen had it in a severe degree. Others who came to London from the West Indies in merchantmen in the end of September were attacked by influenza in their lodgings in the beginning of October.
Doctors at the time could not agree as to how the disease was transmitted, some thinking it was the atmosphere due to a change in the weather, whilst others thought that it was a contagious disease. For a contemporary perspective on the transmission, symptoms and treatment of influenza see Theophilus Thompson “Annals of Influenza” and the example given below, from Dr. Gray’s account in the said work:
Different opinions have been entertained respecting the manner in which this disease was produced and propagated. Some physicians thought it arose solely from the state of the weather in other words, that it was a common catarrh, occasioned as that complaint frequently is, by changes in the sensible qualities of the atmosphere, such as the increase of cold, or moisture and consequently, they supposed it unconnected with any disorder that had prevailed, or did at that time prevail in any other part. Others, admitted its cause to be a particular and specific contagion, totally different from, and independent of, the sensible qualities of the atmosphere, yet thought that cause was conveyed by, and resided in the air. But the greatest number concurred in opinion, that the influenza was contagious, in the common acceptation of that word that is to say, that it was conveyed and propagated by the contact, or at least by the sufficiently near approach, of an infected person.
It appears from the ‘Journal de Médecine,’ that the Faculté de Médecine in Paris were of the first opinion; at their Prima Mensis, the cause of La Grippe, as the epidemic was commonly called, is ascribed to, ‘Les variations de l’ atmosphere.’
At Venice, several physicians ridiculed the common name of the disease (Russian catarrh), and thought the changes of the weather sufficient to account for it, observing in support of their opinion, that the thermometer had sunk no less than ten degrees of Reaumur’s scale (more than 22 of Fahrenheit’s), between the 17th and 19th of July, about which time the disorder first appeared at that place. Other Italian physicians, however, were of a contrary opinion and one (the Chevalier Rosa, of Modena,) has published a treatise upon it, in which, it is said, he strongly and ably contends, that it was contagious.
Notwithstanding the extensive spread of the disease, it was not a severe epidemic and very few people succumbed:
… of those who died, the greater part were old, asthmatic, or who had been debilitated by some previous indisposition.
It is an interesting supposition that had they not died in the influenza epidemic, they may have been killed by the Laki dry fog the following year.
In part 4 – more diseases ….
See also:

Categories: Uncategorized












1 reply »